Overview
Stereotactic radiosurgery (SRS) was conceived by a team of neurosurgeons and physicists in Sweden about 50 years ago to deliver radiation to precise targets in the brain while minimizing injury to adjacent areas.
It uses sophisticated, 3-D-computerized imaging to precisely focus photon beams, delivering a highly-concentrated dose of radiation to a precise target in a single session. Stereotactic radiosurgery is not surgery, in the conventional sense, because there is no incision involved and general anesthesia is not required for adults. SRS works by distorting and destroying the DNA of tumor cells, much the same way as other forms of radiation. As a result, these cells lose their ability to reproduce and die.
Staged radiosurgery, also known as fractionated stereotactic radiosurgery (FSR), is a process in which the total dose of stereotactic radiation is divided into several smaller doses of radiation, on separate days of treatment. Typically, this consists of two to five treatments. In some cases, staged treatment effectively kills the tumor while seemingly decreasing potential side effects compared with single-dose radiosurgery.
In order to precisely direct the radiation beams, a frame is placed on the patients head. Local anesthetic is administered, and the frame is secured to the skull by four sterile pins; the only discomfort is during the administration of the local anesthetic. The pins themselves do not cause pain if the area is well anesthetized. Additional analgesic medication, such as morphine, may be administered intravenously to facilitate patient comfort during the procedure.
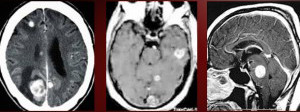
A CT scan is obtained with contrast administration and is then merged or fused with an MRI of the brain that is usually obtained prior to the procedure. The CT complements the MRI, and together, the two studies improve the accuracy of the procedure. Children, or in some rare cases, adults, may require general anesthesia to perform this procedure in which case an anesthesiologist is present throughout. The treatment team is comprised of a number of specialized medical professionals: a radiation oncologist, neurosurgeon, medical radiation physicist, dosimetrist, radiation therapist and a radiation therapy nurse.
The neurosurgeon and radiation oncologist are the primary caregivers and are responsible for the safe and effective administration of radiation and completion of the procedure. They analyze the images and formulate a radiation plan with the rest of the team. Once finalized, the radiation is administered. The patient simply has to lie on a table, much like in a CT scanner, and the head frame is fixed securely to an apparatus on the table, where the radiation beams are precisely directed. Generally, treatment time for one tumor or lesion is in the range of 30 minutes — when more than one tumor is targeted, it may take longer. At the conclusion of the procedure, the frame is removed, a clean dressing is applied on the pin sites and the patient is discharged in the care of a family member or friend.
Steroid medication in the form of Decadron may be administered prior to the procedure and then continued for a brief period of time following the procedure. A routine follow-up with the neurosurgeon and radiation oncologist is generally set up. Additionally, a follow-up MRI of the brain is scheduled at the three-month mark to assess its effectiveness.
TREATMENT + CARE
Treatment Uses
The alternative for patients with more than four metastatic tumors in the brain is known as whole-brain radiation therapy. While this is effective at killing tumor cells and providing this coverage to the entire brain, it can also affect normal brain cells and cause cognitive and intellectual decline; hence, it is reserved for those circumstances in which SRS is not an option.
In some instances, SRS may be used to supplement or boost the effects of whole-brain radiation. In other instances, SRS is advisable but the location of a tumor may be in close proximity to a critical structure, such as the optic nerves; in such cases, the radiation may be divided into fractions and delivered in the same precise targeted manner. This is known as stereotactic radiotherapy (SRT), rather than SRS. The other difference between SRT and SRS is that with SRT, a mask made of a thermoplastic material may be used instead of the frame since the patient has to undergo several sessions of treatment.
Generally, SRS is reserved for tumors that are less than three centimeters in maximal diameter. The most common application of SRS in practice is for the treatment of metastatic brain tumors. Another very common application where SRS is very effective is in the treatment of small tumors arising from the vestibular nerve known as vestibular schwanomma (or acoustic neuroma).
Stereotactic radiosurgery is also a noninvasive treatment option for many patients with conditions such as: arteriovenous malformations (AVMs), arteriovenous fistulas, trigeminal neuralgia and various intracranial tumors.
Arteriovenous Malformations and Arteriovenous Fistulas
An AVM is a tangle of abnormal and poorly formed blood vessels (arteries and veins) with a higher rate of bleeding than normal vessels. AVMs can occur anywhere in the body, but brain AVMs present substantial risks when they bleed. Dural AVMs occur in the covering of the brain and are an acquired disorder that may be triggered by an injury.
An arteriovenous fistula (AVF) is an abnormal channel or passage between an artery and a vein that causes a disruption of normal blood flow patterns. A person may be born with a congenital AVF or may develop an acquired fistula after birth, often caused by an injury that damages the arteries.
Although the effects of SRS on tumor tissue can be seen a few weeks after the procedure, it may take up to two years to see the effects of SRS on an AVM. When SRS is used to treat an AVM, an angiogram is obtained to improve the accuracy targeting the critical portions of the lesion. With AVMs, the nidus, or most concentrated portion of the AVM, is the critical target. It is preferable to keep the size of the target less than 3.5 centimeters. If the AVM nidus is larger, then SRS may be divided into more than one session to avoid complications. Another distinction with AVMs is that in some instances, prior to SRS, embolization of the AVM may be performed to reduce the blood flow within it.
Intracranial Tumors
Stereotactic radiosurgery may be a treatment option for select patients with some metastatic brain tumors that arise from other parts of the body (such as the lungs) and also for the following primary brain tumors:
- Anaplatic astrocytomas
- Chordomas
- Craniopharyngiomas
- Glioblastomas
- Gliomas
- Hemangioblastomas
- Meningiomas
- Pineal tumors
- Pituitary adenomas
- Vestibular schwannomas (acoustic neuromas)
Stereotactic radiosurgery works in the same way as other forms of radiation treatment. The tumor is not removed, but radiation distorts the DNA of the tumor cells. As a result, these cells lose their ability to reproduce. Following treatment, benign tumors may shrink over a period of 18 months to two years. Malignant and metastatic tumors may shrink more rapidly, sometimes within a couple of months.
Meningiomas
Meningioma is another tumor type that responds well to SRS. While surgery is the optimal treatment for meningiomas, those that involve critical structures, such as the cavernous sinus, or those that are located in areas of the brain where safe surgery to remove them is not possible, SRS has a useful role. It can also be used to treat any residual meningioma following surgery, especially if there is growth observed in that tumor remnant. In select cases, with careful consultation between the physicians caring for a patient, SRS may be used for primary brain tumors, such as gliomas, especially when they recur following standard radiation or chemotherapy.
Trigeminal Neuralgia
Trigeminal neuralgia (or tic douloureux) is sometimes described as the most excruciating pain known to humanity. The pain typically involves the lower face and jaw, although sometimes it affects the area around the nose and above the eye. This intense, stabbing, electric shock-like pain is caused by irritation of the trigeminal nerve, which sends branches to the forehead, cheek and lower jaw. It is usually limited to one side of the face.
Stereotactic radiosurgery delivers a single, highly concentrated dose of ionizing radiation to a small, precise target at the trigeminal nerve root. Over a period of time and as a result of radiation exposure, the slow formation of a lesion in the nerve interrupts transmission of pain signals to the brain. It is, however, critical that the procedure be done by a team experienced with this application of SRS, as the target is at the brainstem and there is a risk of injury, given the high dose of radiation used.
Complications
Complications from radiosurgery are few — pin-site bleeding or infection is rare, and swelling around a tumor may occur, which is why Decadron is administered. In rare instances, a seizure may occur; these are generally brief and self-limiting. Caregivers or family members are asked to simply make sure the patient is safe, to call 911 with their physician’s information and to bring them to the hospital for further care. An anti-seizure medication is administered and is usually quite effective in controlling any further seizures.
One late complication that may be seen is known as radiation necrosis: tumor cells killed by radiation but inadequately cleared by the body. In some instances, this can cause further brain swelling requiring additional or increased dose Decadron. In refractory cases, hyperbaric oxygen may be administered, or surgery considered to remove dead tissue. This is why it is important to have close follow-up with a neurosurgeon or radiation oncologist.
It is also possible for a tumor to recur in a different part of the brain, as SRS only targets a very focal area; in such instances, the SRS treatment may be repeated on the new areas of tumor growth. Due to limitations imposed by overlap of radiation beams coming in from different directions, it is generally recommended to limit the number of tumors treated in one session to four. At times, a neurosurgeon and radiation oncologist will extend that number but only with careful consultation and consideration for the patient’s age, tumor type, location of the tumors in the brain and prior treatment history.
Other Uses
At some centers, patients who have Parkinson’s disease, epilepsy or some form of psychoneurosis (such as obsessive compulsive disorder) may be treated on an experimental basis with stereotactic radiosurgery. More recently, with the advent of frameless techniques, stereotactic radiosurgery is being used for spine lesions, more frequently metastatic lesions and less often, benign spine tumors.
Types of Stereotactic Radiosurgery Procedures
Different modalities are available to deliver SRS. The most commonly used ones are the Gamma Knife and LINAC (Linear Accelerator) based systems, such as the CyberKnife® or X-Knife®. Each of these systems has advantages and disadvantages — but they share certain similarities — they all employ a radiation source, or generator, in order to deliver photons to a target and they use computerized algorithms and head frames (or custom-fitted thermoplastic masks) to deliver the radiation precisely.
Gamma Knife
After doctors attach a stereotactic frame to the patient’s head with pins, CT or CAT scan and MRI are used to determine the precise location of the tumor in the patient’s brain. Lesions from 5-40 millimeters can be treated with the Gamma Knife procedure. If the patient has an AVM, an angiogram and a CT scan are performed with the frame attached. The Gamma Knife consists of a sphere containing 201 Cobolt-60 sources, which are positioned so that the beams are targeted toward the patient’s head. The patient’s head is placed within a cavity in the instrument and covered by a helmet that narrows the beams, shielding the head from unwanted radiation. The radiation is controlled by the percentage of the 201 ports that are used, the number of exposures and the head position. Computer-guided dosimetry is specified to match the lesion. Different beam sizes are available by using different helmets with holes of various sizes. Lesions from 5-40 millimeters can be treated. Surgeons can perform multiple exposures by readjusting the helmet and head position to achieve different lesion shapes. This procedure takes approximately 30 minutes.
Linear Accelerator.
The initial steps in the Linear Accelerator (LINAC) procedure are similar to those in the Gamma Knife method. Doctors attach a stereotactic frame to the patient’s head with pins, then use a CT, CAT scan or MRI to determine the precise location of the tumor in the patient’s brain. Lesions up to 3.5 centimeters in diameter can be treated with the LINAC procedure. If the patient has an AVM, an angiogram and a CT scan are performed with the frame attached. Computer-guided dosimetry is specified to match the lesion. A cone that approximates the size of the lesion is placed in the collimator of the linear accelerator. Cones range in size from 12.5 millimeters to 40 millimeters.
The patient is placed lying on his or her back on the treatment couch of the linear accelerator. The head is secured to prevent movement during treatment. Radiation is targeted at the lesion from different directions in the form of arcs. The arc delivers a predetermined amount of radiation, and then the treatment couch is rotated along with the collimator housing the cone. This sequence continues until the therapy is complete. The number of arcs used varies from at least four to six, and the treatment takes approximately 30 minutes. Some devices, such as the CyberKnife, do not use frames, but hold the head in place using masks instead.
Multiple manufacturers make this type of machine, which have brand names such as Peacock®, X-Knife, CyberKnife, Clinac®, etc.
Different health-care centers have different systems, and their efficacy in the treatment of the tumors and lesions mentioned above is similar. In some health-care centers, proton-beam therapy may be available. This is a sophisticated form of radiation that uses similar precision targeting as the other systems mentioned above. However, it uses protons rather than photons. Protons have different physical properties compared to photons — for some tumors, this may be an advantage and referral to a proton beam therapy center is an option.
However, the biological effectiveness of protons is similar to photons and for most brain tumors, standard photon beam therapy is effective, has an excellent track record and is the modality used.
Benefits of SRS
This technology makes it possible for neurosurgeons to reach the deepest recesses of the brain and correct disorders not treatable with conventional surgery. Since there is no incision, there are minimal surgical risks and little discomfort. Adult patients may be lightly sedated but are awake throughout the procedure. Hospitalization is short and at most, requires an overnight stay. The majority of patients are treated on an outpatient basis. As a result, patients experience less discomfort and have much shorter recovery periods than having undergone conventional surgery.
PREVENT + MANAGE
Recovery
Following stereotactic radiosurgery, bandages are placed over the pin sites from the stereotactic frame, and the bandages should be removed the following day. Patients may be observed for a specified time after the treatment before they go home, or they may be kept in the hospital overnight for observation. Some people experience minimal tenderness around the pin sites. Occasionally, swelling also may occur around the pin sites. Most patients can return to their usual activities the following day if swelling is not bothersome.
Follow-up
Each situation must be carefully individualized with close consultation between the patient, the neurosurgeon and radiation oncologist, which is essential in order to decide upon the best treatment plan. Customarily, the neurosurgeon will want to see the patient in the office about one month after the procedure. A neurological examination will be performed. Often, a diagnostic test, such as a CT scan or MRI, will be performed about six months after the procedure to check on the status of the radiated area. These changes may need between one to three years to take effect.
Resources
- Evidence-based Guidelines for Stereotactic Radiosurgery: Status and Future Directions, AANS Neurosurgeon
- Image-guided Volumetric Stereotactic Removal of Tumors, AANS Neurosurgeon
- The Genesis of Image-guided Radiation, AANS Neurosurgeon
Note from AANS
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon online tool.
