OVERVIEW
The neck is part of a long flexible column, known as the spinal column or backbone, which extends through most of the body. The cervical spine (neck region) consists of seven bones (C1-C7 vertebrae), which are separated from one another by intervertebral discs. These discs allow the spine to move freely and act as shock absorbers during activity.
Attached to the back of each vertebral body is an arch of bone that forms a continuous hollow longitudinal space, which runs the whole length of the back. This space, called the spinal canal, is the area through which the spinal cord and nerve bundles pass. The spinal cord is bathed in cerebrospinal fluid (CSF) and surrounded by three protective layers called the meninges (dura, arachnoid, and pia mater).
At each vertebral level, a pair of spinal nerves exit through small openings called foraminae (one to the left and one to the right). These nerves serve the muscles, skin and tissues of the body and thus provide sensation and movement to all parts of the body. The delicate spinal cord and nerves are further supported by strong muscles and ligaments that are attached to the vertebrae.
Cervical Stenosis
Cervical stenosis occurs when the spinal canal narrows and compresses the spinal cord and is most frequently caused by aging. The discs in the spine that separate and cushion vertebrae may dry out and herniate. As a result, the space between the vertebrae shrinks, and the discs lose their ability to act as shock absorbers. At the same time, the bones and ligaments that make up the spine become less pliable and thicken. These changes result in a narrowing of the spinal canal. In addition, the degenerative changes associated with cervical stenosis can affect the vertebrae by contributing to the growth of bone spurs that compress the nerve roots. Mild stenosis can be treated conservatively for extended periods of time, as long as the symptoms are restricted to neck pain. Severe stenosis requires referral to a neurosurgeon.
Age, injury, poor posture or diseases such as arthritis can lead to degeneration of the bones or joints of the cervical spine, causing disc herniation or bone spurs to form. Sudden severe injury to the neck may also contribute to disc herniation, whiplash , blood vessel destruction, vertebral bone or ligament injury and, in extreme cases, permanent paralysis. Herniated discs or bone spurs may cause a narrowing of the spinal canal or the small openings through which spinal nerve roots exit.
SYMPTOMS + TYPES
Neck pain may be caused by disc degeneration, narrowing of the spinal canal, arthritis and, in rare cases, cancer or meningitis . Symptoms include:
- Neck or arm pain
- Numbness and weakness in the upper extremities hands
- Unsteady gait when walking
- Muscle spasms in the legs
- Loss of coordination in arms, hands, finger
- Loss of muscle tone in arms and/or hands
- Dropping items or loss of dexterity of hands
When & How to Seek Medical Care
You should consult a neurosurgeon for neck pain if you have the above listed symptoms or the following:
- Neck pain after an injury or blow to the head or neck
- Fever or headache accompanies the neck pain
- Stiff neck prevents touching chin to chest
- Progression of weakness or numbness of arms and/or legs
- Pain not improving after conservative management
For serious neck problems, a primary care physician and often a specialist, such as a neurosurgeon, should be consulted to make an accurate diagnosis and prescribe treatment. If you experience sudden onset of weakness, the situation may be emergent and you must seek medical attention at an emergency room, as delaying care may lead to permanent neurological injury.
For more gradual onset of symptoms over weeks to months, see your primary care physician for potential referral to a spine surgeon.
TESTING + DIAGNOSIS
Diagnosis is made by a neurosurgeon based on history, symptoms, a physical examination and results of tests, including the following. As some degree of arthritis and spinal degeneration is normal due to aging, the neurosurgeon must determine if findings on imaging studies correlate to symptoms.
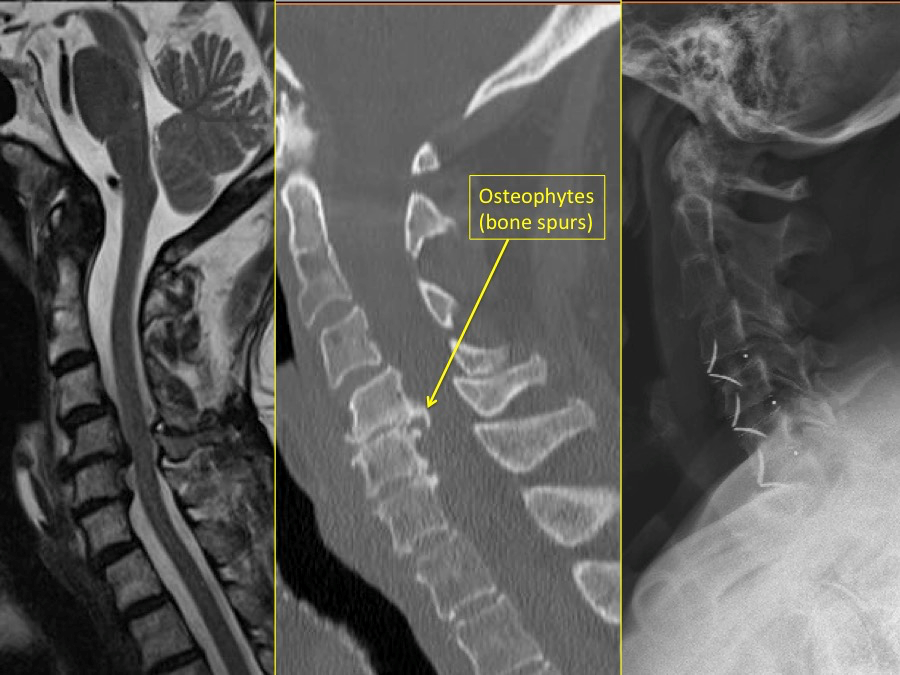
- Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads and combines a multitude of thin-cut X-rays that can show the shape and size of the spinal canal, its contents and the structures around it, especially bones. The CT scan gives the neurosurgeon information about abnormalities of the bones, such as bone spurs, osteophytes, presence of fusion and bone destruction due to infection or tumor.
- Electromyogram and Nerve Conduction Studies (EMG/NCS): These tests measure the electrical impulse along nerve roots, peripheral nerves and muscle tissue. This will indicate whether there is ongoing nerve damage, if the nerves are in a state of healing from a past injury or whether there is another site of nerve compression.
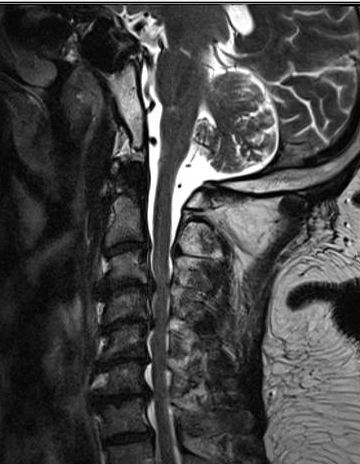
- Magnetic resonance imaging (MRI): A diagnostic test that produces images of body structures using powerful magnets and computer technology; can show the spinal cord, nerve roots and surrounding areas as well as enlargement, degeneration, disc herniations, infections and tumors.
- Myelogram: An X-ray of the spinal canal following injection of contrast material into the surrounding cerebrospinal fluid spaces; can show pressure on the spinal cord or nerves due to herniated discs, bone spurs or tumors.
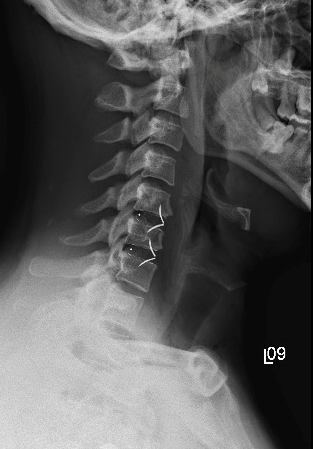
- X-rays: X-rays can show the boney structures of the spine. This provides information on spinal alignment, presence of arthritis, disc degeneration and fractures. X-rays are utilized as a relatively low risk postoperative imaging study to monitor the spine and any instrumentation placed.

TREATMENT + CARE
Non-Surgical Treatments
Nonsurgical treatment is the first approach in patients with common neck pain not involving trauma. For example, many patients with cervical disc herniations improve with conservative treatment and time and do not require surgery. Conservative treatment includes time, medication, brief bed rest, reduction of strenuous physical activity and physical therapy. A doctor may prescribe medications to reduce the pain or inflammation and muscle relaxants to allow time for healing to occur. An injection of corticosteroids into the joints of the cervical spine or epidural space be used to temporarily relieve pain.
Surgery
The patient may be a candidate for surgery if:
- Conservative therapy is not helping
- Presence of progressive neurological symptoms involving arms and/or legs
- Difficulty with balance or walking
- In otherwise good health
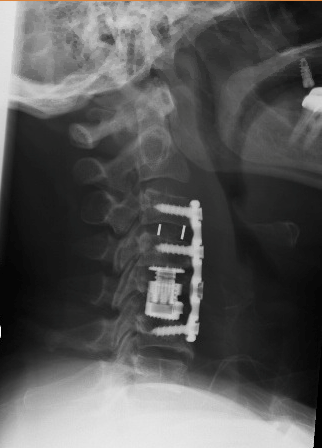
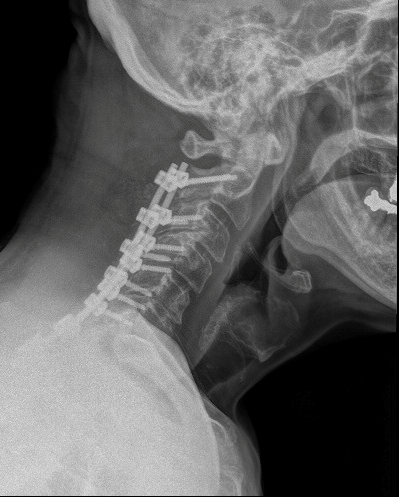
There are several different surgical procedures that can be utilized, the choice of which is influenced by the specifics of each case. In a percentage of patients, spinal instability may require that spinal fusion be performed, a decision that is generally determined prior to surgery. Spinal fusion is an operation that creates a solid union between two or more vertebrae. Various devices (like screws or plates) may be used to enhance fusion and support unstable areas of the cervical spine. This procedure may assist in strengthening and stabilizing the spine and may thereby help to alleviate severe and chronic neck pain.
No matter which approach is taken, the goals of surgery are the same:
- Decompress the spinal cord and/or nerves
- Maintain or improve stability of the spine
- Maintain or correct the spinal alignment
Anterior Cervical Discectomy
This operation is performed on the neck to relieve pressure on one or more nerve roots or on the spinal cord. The cervical spine is reached through a small incision in the anterior (front) of the neck. If only one disc is to be removed, it will typically be a small horizontal incision in the crease of the skin. If the operation is more extensive, it may require a slanted or longer incision. After the soft tissues of the neck are separated, the intervertebral disc and bone spurs are removed and the spinal cord and nerve roots are decompressed. The space left between the vertebrae is filled with a small piece of bone or device through spinal fusion. In time, the vertebrae will fuse or join together across that level.
Anterior Cervical Corpectomy
The corpectomy is often done for cervical stenosis with spinal cord compression caused by bone spur formations that cannot be removed with a discectomy alone. In this procedure, the neurosurgeon removes a part or all of the vertebral body to relieve pressure on the spinal cord. One or more vertebral bodies may be removed, including the adjoining discs for multilevel disease. The space between the vertebrae is filled using a small piece of bone or device through spinal fusion. Because more bone is removed, the recovery process for the fusion to heal and the neck to become stable is generally longer than with anterior cervical discectomy. The surgeon may choose to support the anterior construct with posterior instrumentation and fusion, depending on the amount of spinal reconstruction required.
Posterior Microdiscectomy
This procedure is performed through a small vertical incision in the posterior (back) of your neck, generally in the middle. This approach may be considered for a large soft disc herniation that is located on the side of the spinal cord. A high speed burr is used to remove some of the facet joint, and the nerve root is identified under the facet joint. The nerve root needs to be gently moved aside to free up and remove the disc herniation.
Posterior Cervical Laminectomy and Fusion
This procedure requires a small incision in the middle of the back neck to remove the lamina. Removal of the bone is done to allow for removal of thickened ligament, bone spurs or disc material that may be pushing on the spinal cord and/or nerve roots. The foramen, the passageway in the vertebrae through which the spinal nerve roots travel, may also be enlarged to allow the nerves to pass through. Depending on the severity of the degeneration and amount of reconstruction required, the surgeon may determine that a posterior spinal fusion is needed in addition to the laminectomy to maintain proper spinal stability and alignment. This may reduce the risk of requiring future interventions at those levels.
Risks and Outcome
Although complications are fairly rare, as with any surgery, the following risks may be associated with cervical spine surgery:
- Infection
- Chronic neck or arm pain
- Inadequate symptom relief
- Damage to the nerves and nerve roots
- Damage to the spinal cord (about 1 in 10,000), resulting in paralysis
- Spinal instability
- Damage to the esophagus, trachea or vocal cords from anterior approach
- Injury to the carotid or vertebral arteries, which could result in stroke from anterior approach
- Fusion that does not occur – pseudarthrosis
- Instrumentation breakage and/or failure
- Persistent swallowing or speech disturbance
- Leakage of cerebral spinal fluid
Follow-up
The doctor will give specific instructions post-surgery and usually prescribe pain medication. The doctor will help determine when the patient can resume normal activities such as returning to work, driving and exercising depending on the type of surgery. Some patients may benefit from supervised rehabilitation or physical therapy after surgery. Discomfort is expected while the patient gradually returns to normal activity, but pain is a warning signal that he or she might need to slow down.
Postoperatively, the neurosurgeon may elect to obtain x-rays of the spine to assess alignment, status of the instrumentation and fusion and generally monitor levels of the spine adjacent to the surgery.
Case: Cervical stenosis
Note from AANS
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon”online tool.
