Overview
Cushing’s syndrome is a disorder caused by the body’s exposure to an excess of the hormone cortisol. Cortisol affects all tissues and organs in the body. These effects together are known as Cushing’s syndrome.
Cushing’s syndrome can be caused by overuse of cortisol medication, as seen in the treatment of chronic asthma or rheumatoid arthritis (iatrogenic Cushing’s syndrome), excess production of cortisol from a tumor in the adrenal gland or elsewhere in the body (ectopic Cushing’s syndrome) or a tumor of the pituitary gland secreting adrenocorticotropic hormone (ACTH) which stimulates the over-production of cortisol from the adrenal gland (Cushing’s disease).
Cortisol is a normal hormone produced in the outer portion of the adrenal glands. When functioning correctly, cortisol helps the body respond to stress and change. It mobilizes nutrients, modifies the body’s response to inflammation, stimulates the liver to raise blood sugar and helps control the amount of water in the body. Cortisol production is regulated by the ACTH produced in the pituitary gland.
Prevalence of Cushing’s Syndrome
- An estimated 10-15 per million people are affected every year.
- Pituitary adenomas (Cushing’s disease) account for more than 70 percent of cases in adults and about 60-70 percent of cases in children and adolescents.
- Cushing’s syndrome most commonly affects adults ages 20-50 and is more prevalent in females, accounting for about 70 percent of all cases.
Underlying Causes
Pituitary Adenomas — Cushing’s Disease
Pituitary adenomas are benign tumors of the pituitary gland that secrete increased amounts of ACTH causing excessive cortisol production. Most patients have a single adenoma. First described in 1912 by neurosurgeon Harvey Cushing, MD, in his book The Pituitary Body and Its Disorders, Cushing’s disease is the most common cause of spontaneous Cushing’s syndrome, accounting for 60-70 percent of all cases.
Ectopic ACTH Syndrome
Some benign or malignant (cancerous) tumors that arise outside the pituitary gland can produce ACTH. This condition is known as ectopic ACTH syndrome. Lung tumors (malignant adenomas or carcinoids) cause more than 50 percent of these cases. Other less common types of tumors that can produce ACTH are thymomas, pancreatic islet cell tumors and medullary carcinomas of the thyroid.
Adrenal Tumors
An abnormality of the adrenal glands, such as an adrenal tumor, may cause Cushing’s syndrome. Most of these cases involve non-cancerous tumors called adrenal adenomas, which release excess cortisol into the blood.
Adrenocortical carcinomas, or adrenal cancers, are the least common cause of Cushing’s syndrome. Cancer cells secrete excess levels of several adrenal cortical hormones including cortisol and adrenal androgens. Adrenocortical carcinomas often cause very high hormone levels and a rapid onset of symptoms.
Familial Cushing’s Syndrome
Most cases of Cushing’s syndrome are not genetic. However, some individuals may develop Cushing’s syndrome due to an inherited tendency to develop tumors of one or more endocrine glands. In primary pigmented micronodular adrenal disease, children or young adults develop small cortisol-producing tumors of the adrenal glands. In multiple endocrine neoplasia type I (MEN I), hormone-secreting tumors of the parathyroid glands, pancreas and pituitary gland can occur. Cushing’s syndrome in MEN I may be due to a pituitary, ectopic or adrenal tumor.
Symptoms
- Weight gain in face (moon face)
- Weight gain above the collar bone (supraclavicular fat pad)
- Weight gain on the back of neck (buffalo hump)
- Skin changes with easy bruising in the extremities and development of purplish stretch marks (striae) particularly over the abdomen or axillary region
- Red, round face (plethora)
- Central obesity with weight gain centered over the chest and abdomen with thin arms and legs
- Excessive hair growth (hirsutism) on face, neck, chest, abdomen and thighs
- Female balding
- Generalized weakness and fatigue
- Blurry vision
- Vertigo
- Muscle weakness
- Menstrual disorders in women (amenorrhea)
- Decreased fertility and/or sex drive (libido)
- Hypertension
- Poor wound healing
- Diabetes mellitus
- Severe depression
- Extreme mood swings
TESTING + DIAGNOSIS
The diagnosis of Cushing’s syndrome is based on clinical suspicion combined with a review of the patient’s medical history, physical examination and laboratory tests to help determine the existence of excessive levels of cortisol. A patient suspected of having Cushing’s syndrome must initially have an appearance suggestive of excess cortisol production combined with an elevated 24-hour urinary excretion of cortisol. In assessing the physical features of Cushing’s syndrome, it can often be beneficial to compare old and recent photographs to reveal the classic changes in facial and body appearance associated with this disorder.
The following tests can help determine if there are excessive levels of cortisol being produced:
- The 24-hour urinary cortisol test measures the amount of cortisol being produced within the urine over the course of an entire day. Levels higher than 50-100 micrograms per day in an adult suggest the presence of Cushing’s syndrome. Although the majority of patients with Cushing’s syndrome have elevated levels of cortisol, it is becoming increasingly evident that many patients with a mild case of Cushing’s syndrome may also have normal levels of cortisol resulting in several 24-hour urine collections to confirm a diagnosis.
- The low-dose dexamethasone suppression test measures the response of the adrenal glands to ACTH and has been widely utilized for four decades. It involves taking a small dose of a cortisol-like drug, dexamethasone (1 mg), at 11 p.m., then having blood drawn to screen for cortisol the following morning. In patients without Cushing’s syndrome, the morning level of cortisol is typically very low, indicating that ACTH secretion was suppressed by the evening dose of dexamethasone. In patients with Cushing’s syndrome, the morning cortisol level will be high. It is evident that normal patients will suppress their cortisol to a very low level (1.8 mg/dl), whereas those suffering from Cushing’s syndrome will not. Using this strict criterion, this test should provide an estimated 95-97 percent diagnostic accuracy rate. However, some patients with a mild case of Cushing’s syndrome can suppress their cortisol to low levels making it difficult to fully diagnose utilizing this test.
- The late-night salivary cortisol test is a relatively new test that checks for elevated levels of cortisol in the saliva between 11 p.m. and midnight. Cortisol secretion is usually very low late at night, but in patients with Cushing’s syndrome, the level will always be elevated during this time. Collection of saliva requires special sampling tubes; however, this is an easy test for patients to perform and can be done multiple times. Normal levels of late-night salivary cortisol virtually exclude the diagnosis of Cushing’s syndrome. When administered correctly, this test should provide an estimated 93-100 percent diagnostic accuracy rate.
After a definitive diagnosis has been made, the source must then be determined. The first step in distinguishing the underlying cause is the measurement of ACTH. Patients with ACTH-secreting tumors will either have a normal or elevated level of ACTH. In contrast, patients with an excess of adrenal cortisol will have a subnormal level. Performing a high-dose dexamethasone suppression test may be helpful in this situation. This test, similar to the low-dose dexamethasone suppression test, involves taking a high dose of dexamethasone (8 mg) at 11 p.m. then having blood drawn to screen for the presence of cortisol the following morning. In normal patients, the morning level of cortisol will again be very low. Patients with pituitary tumors will also suppress their serum cortisol level, but those with adrenal tumors will maintain a high level of cortisol production. A high level of cortisol points to a non-pituitary source.
Despite the tests described above, distinguishing a pituitary from a non-pituitary ACTH-secreting tumor can be diagnostically challenging. The majority of patients with ACTH-secreting tumors have a pituitary lesion that is often very small.
The following tests are recommended:
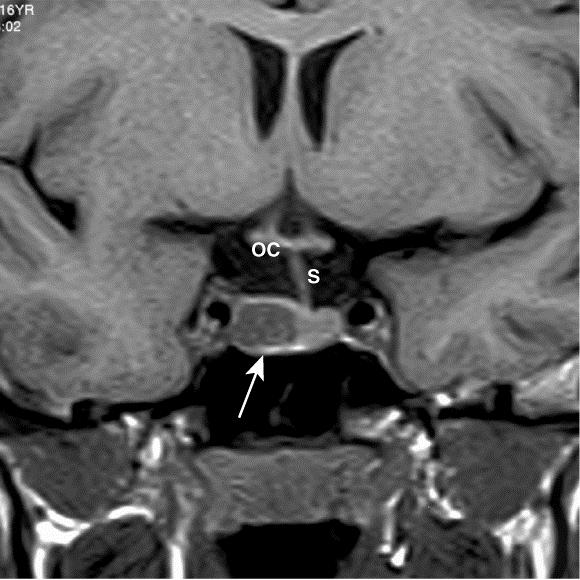
- Magnetic Resonance Imaging (MRI) of the pituitary gland with gadolinium enhancement is a recommended approach. When an obvious pituitary tumor (>5 mm) is identified with an MRI, further diagnostic evaluation may not be needed depending on the clinical presentation. However, about 50 percent of patients will have a “normal” MRI of the pituitary, with 10 percent having incidental tumors unrelated to ACTH production. In such cases, the MRI will not provide a definitive diagnosis and additional tests will be required.
- Petrosal sinus sampling is a test used to distinguish the source of ACTH secretion and should only be performed after the diagnosis of Cushing’s syndrome has been confirmed. ACTH and other pituitary hormones produced in the pituitary gland enter the blood stream by drainage through veins called the inferior petrosal sinuses. To perform this procedure, a catheter is placed in both veins at the same time and blood is sampled for ACTH before and after the administration of the corticotropin-releasing hormone (CRH) and at two, five and 10 minute intervals. This invasive technique should be performed at a medical center by a medical professional with extensive experience in this procedure. When administered correctly, this test should provide an estimated 95-98 percent diagnostic accuracy rate.
Treatment of Cushing’s Syndrome
Treatment of Cushing’s syndrome depends on the underlying cause of excess cortisol but may perhaps include surgery, radiation, chemotherapy or the use of cortisol-inhibiting drugs. If the cause is iatrogenic, from long-term use of glucocorticoid hormones to treat another disorder, the physician will gradually reduce the dose of the externally administered steroid to the lowest dose adequate for control of that disorder. Once control is established, the dose of glucocorticoid hormones may be given on alternate days to lessen side effects for the patient.
Treatment of Cushing’s Disease
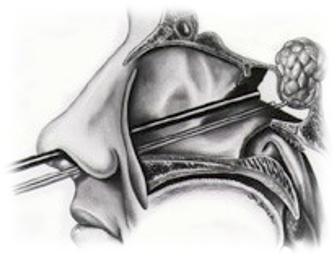
Microsurgical resection of an ACTH-secreting pituitary adenoma is the optimum treatment for Cushing’s disease with cure rates of 80-90 percent if a tumor is found. Surgery is most often done through a transnasal transsphenoidal approach, which will not leave a visible scar. This type of surgery may be performed, per the surgeon’s preference, using either a minimally invasive operating microscope or with the use of an endoscope. Partial removal of the pituitary gland (subtotal hypophysectomy) may be used in patients without clearly identifiable adenomas.
In patients to whom a remission is not obtained after surgery, the use of various medications that can inhibit cortisol production may be used, such as:
- Ketoconazole (Nizoral)
- Mitotane (Lysodren)
- Metyrapone (Metopirone)
- Mifepristone (Korlym)
These agents are not as effective as surgery and are considered a second–line course of treatment. In some patients who are particularly resistant to all forms of therapy, removal of the adrenal glands bilaterally (bilateral adrenalectomy) may be considered.
Post-surgery, with successful tumor removal, the production of ACTH drops below normal. This decrease is natural and temporary, and patients are prescribed a synthetic form of cortisol such as hydrocortisone or prednisone to compensate this change. Most patients can discontinue replacement therapy within six to 12 months, but others may require the use of oral steroids for several years to, possibly, their lifetime. Patients who need adrenal surgery may also require steroid replacement therapy.
One additional treatment option in patients who have failed surgical procedures or are too high risk medically to bring to surgery is radiation therapy. Radiation therapy, which is administered over a six-week period to the pituitary gland, has yielded improvement in 40-50 percent of adults and up to 85 percent of children.
Stereotactic radiosurgery has also been found to be an effective treatment for patients with ACTH-secreting pituitary adenomas. A recent study demonstrated endocrine remission in 54 percent of patients and tumor-growth control in 96 percent. However, ongoing observation is required to monitor for tumor growth, disease recurrence, the development of new hormone deficiencies and damage to the optic pathways and brain.
Resources
- Cushing’s Help and Support
- Cushing’s Support & Research Foundation
- National Endocrine and Metabolic Diseases Information Service
- Pituitary Network Association
Note from AANS
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon online tool.
