OVERVIEW
Intracerebral hemorrhage (bleeding into the brain tissue) is the second most common cause of stroke (15-30% of strokes) and the most deadly.
Blood vessels carry blood to and from the brain. Arteries or veins can rupture, either from abnormal pressure or abnormal development or trauma. The blood itself can damage the brain tissue. Furthermore, the extra blood in the brain may increase the pressure within the skull (intracranial pressure (ICP)) to a point that further damages the brain.
Causes
Hypertension: chronic high blood pressure causes changes to the arteries of the brain which can make them much more likely to rupture.
Age: more common after age of 55, with buildup of protein in walls of arteries called amyloid angiopathy.
Gender: more common in men.
Race: affects African Americans and Asians more than whites; likely related to higher prevalence of Hypertension in those races.
Previous history of stroke: increases risk 23 times.
Alcohol use and street drugs: cocaine, amphetamines increases risk.
Liver disease: increases risk due to issues with blood clotting.
Use of blood thinners.
Primary brain causes: tumors, vascular anomalies, infection and venous sinus thrombosis.
Left: Axial nonenhanced CT scan revealing a spherical homogeneous hyperintense area measuring 7 cm in diameter. The hemorrhage is located primarily in the right temporal lobe and causes 1 cm of midline shift. Right: Digital subtraction angiography demonstrating an 8-mm saccular aneurysm arising from the proximal third of the MMA (arrowhead). In addition, there is obvious displacement of surrounding vessels.
Symptoms
Intracerebral hemorrhage can be characterized by a smooth progressive onset over minutes to hours, but can also be like ischemic stroke, with sudden onset of symptoms. Symptoms depend on location of hemorrhage an include:
- Headache, nausea, vomiting
- Alterations in levels of consciousness
- Weakness/numbness in face, arm or leg (usually on one side)
- Vision loss
- Seizures
When & How to Seek Medical Care
Seek medical care immediately when neurological symptoms occur. Hemorrhages often enlarge within first three hours in at least 33% of cases and volume of hemorrhage correlates highly with outcomes (bigger the hemorrhage, worst the outcome).
Serial computerized tomography (CT) scans in Case 3. An increase in volume of hemorrhage from 8 to 35 cc was recorded between the first CT scans (upper), obtained 50 minutes after onset of symptoms, and the second CT scans (lower), obtained 210 minutes after onset.
Testing & Diagnosis
A non-contrast computer tomography (CT) scan of brain is the diagnostic study of choice. CT or magnetic resonance (MR) angiogram is recommended (once the patient is stabilized).
Some patients may experience delayed deterioration due to re-bleeding, swelling, hydrocephalus (accumulation of fluid due to blood or brain swelling blocking natural drainage pathways) and seizures.
Treatment
Treatment focusses on stopping the bleeding, removing the clot and relieving pressure on the brain. If left alone, the brain will eventually re-absorb the clot. The damage done by increased brain pressure over a long period may be irreversible.
Non-Surgical Treatments
Candidates for non-surgical treatment are patients with:
- Minimal symptoms;
- Minimal chance of a favorable outcome (large hemorrhage, poor neurologic condition, advanced age, bleeding disorder); and
- A hemorrhage location (basal ganglia or thalamic hemorrhage, where surgery is no better than medical management).
Non-surgical treatments include:
- Clotting factor administration, if patient was on blood thinners;
- Blood pressure control to reduce risk of more bleeding; and
- Measuring and controlling ICP (pressure on brain tissue due to clot).
Surgery
Candidates for surgical treatment are patients:
- Less than 50 years of age (tolerate surgery better than an elderly patient);
- With a hemorrhage location in a favorable location for surgical evacuation, including in the lobar, cerebellar, external capsule and non-dominant hemisphere; and
- For whom surgery may lower issues with re-bleeding, edema and necrosis, but rarely causes neurologic improvement.
Surgical treatments include:
- A craniotomy involves removing a piece of the skull bone and exposing the brain to remove the clot. It is useful when the clot is close to the surface of the brain or if the clot is associated with an underlying brain lesion.
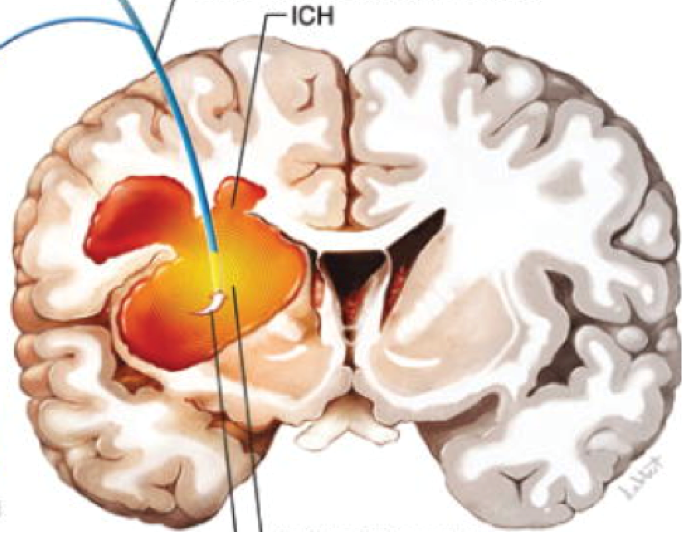
- Stereotactic clot aspiration is a minimally invasive technique to evacuate a clot located deep inside the brain. This is possible with use of neuronavigation technology, which works similar to GPS in cars.
Apparatus for the SLEUTH study. Left: A standard EVD catheter with a small ultrasound-emitting probe (EKOS) inserted in the catheter tip fenestration. Right: Illustration showing stereotactic insertion of the ventricular catheter with the EKOS US microcatheter (upper). The tip of the catheter assembly is seen within the intraparenchymal clot (lower). Printed with permission from the Swedish Neuroscience Institute. (https://thejns.org/focus/view/journals/neurosurg-focus/32/4/2012.1.focus11362.xml)
Follow-up
The ICH score was developed to provide a clinical grading scale for ICH that helps standardize clinical treatment protocols and clinical research studies in ICH. The score was developed at UCSF, with the original study analyzing 161 patients presenting with ICH 1997-98. Overall, the analysis helps provide information about the degree of severity of ICH as well as 30-day mortality rates that helped guide decision-making.
Latest Research
Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral hemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial concluded that Platelet transfusion seems inferior to standard care for people taking antiplatelet therapy before intracerebral hemorrhage. Platelet transfusion cannot be recommended for this indication in clinical practice.
CLEAR-IVH (Clot Lysis: Evaluating Accelerated Resolution of Intraventricular Hemorrhage) trial Phase III – pending results.
Resources for More Information
American Stroke Association. (2020). Hemorrhagic Strokes (Bleeds). Retrieved from https://www.stroke.org/en/about-stroke/types-of-stroke/hemorrhagic-strokes-bleeds
Note from AANS
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information provided is an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon online tool.
