OVERVIEW
When the lumbar (lower) spine is strained or sprained, the muscles and tissues become swollen. This inflammation causes pain and may cause muscle spasms.
Causes
Lumbar (lower back) muscle strains and sprains are the most common causes of low back pain. Muscle strains and sprains are common in the lower back, because it supports the weight of the upper body and is involved in moving, twisting and bending. Lumbar muscle strain is caused when muscle fibers are abnormally stretched or torn. Lumbar sprain is caused when ligaments (the tough bands of tissue that hold bones together) are torn from their attachments. Both of these can result from a sudden injury or from gradual overuse. Lumbar strain or sprain can be debilitating.
Types of Muscles Supporting the Spine
- Extensors (back muscles and gluteal muscles)
- Flexors (abdominal muscles and iliopsoas muscles)
- Obliques or rotators (side muscles)
Symptoms
- Low back pain that may radiate into the buttocks, but does not affect the legs
- Stiffness in the low back area, restricting range of motion
- Inability to maintain normal posture due to stiffness and/or pain
- Muscle spasms either with activity or at rest
- Pain that persists for a maximum of 10-14 days
When & How to Seek Medical Care
If low back pain lasts for longer than one to two weeks, seek medical care. First, make an appointment with your primary care physician.
Seek immediate medical attention if any of the following symptoms are present in addition to back pain:
- Severe abdominal pain
- Unexplained fever (higher than 100.4F or 38.0C)
- Loss of control of your bowels or bladder
Testing & Diagnosis
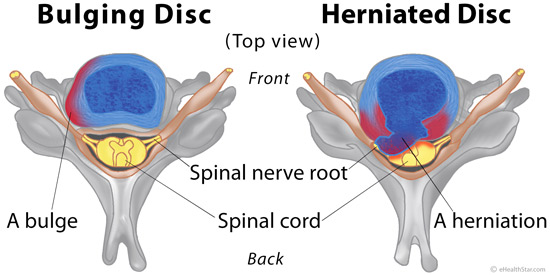
Diagnostic testing is usually not necessary, unless pain has lasted for more than six weeks and has not improved as expected following physical therapy. It is important to rule out underlying causes, such as an undetected disc injury. If symptoms are persistent for longer than six weeks and physical therapy has not improved the condition, the following tests may be ordered by a doctor.
- X-ray: An x-ray produces a picture of a part of the body, and can show the structure of the vertebrae and the outline of the joints. X-rays of the spine are used to search for other potential causes of pain, i.e. infections, fractures, etc.
- Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology; can show the spinal cord, nerve roots and surrounding areas as well as enlargement, degeneration and tumors.
Treatment
Staying active and avoiding bed rest is recommended when experiencing back pain. Bed rest can lead to a loss of muscle strength and may increase muscle stiffness, adding to pain and discomfort. Sprain and strain is commonly treated with nonsteroidal anti-inflammatory medication, if the pain is mild to moderate.
A doctor may recommend physical therapy. The therapist will perform an in-depth evaluation, which, combined with the doctor’s diagnosis, dictates a treatment specifically designed for patients with low back pain. Therapy may include pelvic traction, gentle massage, ice and heat therapy, ultrasound, electrical muscle stimulation and stretching exercises. A physical therapist will also recommend exercises to do regularly at home in the long-term. Alternative holistic options to relieve low back pain include acupuncture, chiropractic care, massage and yoga. Pain medications and muscle relaxants may also be helpful on a short-term basis in combination with the physical therapy.
Follow-up
The likelihood of a complete recovery from a lumbar strain or sprain injury is excellent. More than 90% of patients completely recover from an episode of lumbar muscle strain or sprain within one month. Heat and ice treatment are recommended on an as-needed basis at home to treat sudden flare-ups of low back pain, along with anti-inflammatory medications. However, low back strain may develop into a chronic condition unless efforts are made to change habits that contribute to the problem.
The following tips may be helpful in preventing low back pain associated with strain and sprain:
- Do core strengthening exercises to provide more spine stability in the long-term. Swimming, stationary bicycling and brisk walking are good aerobic exercises that generally do not put extra stress on the back.
- Use correct lifting and moving techniques, such as squatting to lift a heavy object. Do not bend and lift. Get help if an object is too heavy or awkward.
- Maintain correct posture when sitting and standing.
- Quit smoking. Smoking is a risk factor for arthrosclerosis (hardening of the arteries), which can cause lower back pain and degenerative disc disorders.
- Avoid stressful situations, if possible, as this can cause muscle tension.
- Maintain a healthy weight. Extra weight, especially around the midsection, can put strain on the lower back.
Resources for More Information
- Cleveland Clinic. (2018). Back Strains and Sprains. Retrieved from https://my.clevelandclinic.org/health/diseases/10265-back-strains-and-sprains
- NIH. (2019). Low Back Pain Fact Sheet. Retrieved from https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/low-back-pain-fact-sheet
Patient Pages are authored by neurosurgical professionals, with the goal of providing useful information to the public.
Note from AANS
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information provided is an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon online tool.
